INTRODUCTION
Osteoporosis is a chronic disease defined by the deterioration of bone architecture leading to increased bone fragility and susceptibility to pathologic fractures.1 More than 10 million patients living in the United States currently suffer from osteoporosis (National Osteoporosis Foundation 2014).2 Dysregulation in bone physiology leads to abnormal bone architecture driven by aberrant signaling processes, and is often associated with a decrease in estrogen levels in this population.3 Current research suggests that inflammation may play a role in the development of the disease.4 Osteoporosis is a leading cause of hip fractures in the elderly4 which is often associated with early mortality.5 The association between osteoporotic fractures and mortality in this population has prompted the United States Preventive Services Task Force (USPSTF) to establish screening recommendations for women greater than 65 years old with annual bone densitometry.6 Current medical therapy is aimed at slowing bone loss and includes bisphosphonates, a monoclonal antibody, and a selective estrogen receptor modulator (SERM). However, the use of these agents are limited by cost and side effects such as osteonecrosis of the jaw with bisphosphonates and thromboembolic events with SERMs.7
Bone remodeling can be monitored using serum markers such as Osteocalcin (OSCAL), Serum N-telopeptide (SNTX), C-telopeptide (CTX) Bone Specific Alkaline Phosphatase (BSAP), Urinary Hydroxyproline, Bone Sialoprotein, N-terminal Propeptide of Procollagen Type I (P1NP), etc.8 During the first few months of bisphosphonate therapy, P1NP has been shown to decrease significantly, providing support that they are sensitive in monitoring bone turnover in osteoporosis.9
OSCAL and SNTX, the two markers used in this case report are used to monitor bone resorption and remodeling. Osteoblasts generate osteocalcin, which is integrated into the bone matrix during bone formation. OSCAL is used as a measure of bone turnover and not a measure of bone formation.10 Conversely, SNTX is a marker for osteoclastic activity, the initial phase of bone remodeling
Weight-bearing activity (WBA) has been recognized as a conservative modality for slowing bone loss in patients with low BMD prior to considering pharmacotherapy.11 Compliance, availability, cost, and safety are notable limitations.12
CASE REPORT
A 61-year old female with a past history of cervical degenerative disc disease, chronic cervical pain, low bone mineral density (BMD), presented to our outpatient OMT clinic with a complaint of back pain. She had a remote surgical history of cervical decompression with a fusion of C4- C7. Her medications included Oxycodone and Tizanidine. Additionally, she receives bi-annual steroid injections to the cervical spine.
On examination, her vitals were stable, she appeared comfortable, and in no acute distress. She had a thin body habitus. She was able to ambulate independently and easily transition from a standing to a seated, and then to a supine position without assistance.
On osteopathic structural examination, she demonstrated a range of motion restriction in lumbar flexion, extension, side-bending and rotation. Cranial osteopathic examination demonstrated a right torsion cranial strain pattern, a base compression, and a left occipitomastoid suture compression. There was increased muscle hypertonicity noted in the left cervical paraspinal muscles, scalene muscles, sternocleidomastoid, and trapezius and thoracic paraspinal muscles. An “S” shaped structural scoliosis displayed apexes at T6 and L3. Additional somatic dysfunctions noted included left first rib inhalation dysfunction, right ilium rotated anterior, sacroiliac joint compressed on the left. Further examination revealed a tight iliotibial band.
Moreover, her left fibular head was in the posterior position and paravertebral muscle hypertonicity was appreciated at the thoracolumbar junction.
TREATMENT
The patient was treated twice per week for three and a half weeks. Each treatment consisted of five minutes of seated articulatory techniques applied to the thoracic and lumbar spine including both translatory and rotational forces. This was followed by 10 minutes of a vigorous supine pedal pump. These techniques introduced axial compressive forces throughout the spine and skeletal system, which might mimic weight-bearing exercises and simultaneously facilitate lymphatic activity.
To monitor the effects of our treatments we utilized two serum bone turnover markers; osteocalcin and N- Telopeptide. Serum markers are a quick, simple method to evaluate the response to our treatment. In clinical practice, bone turnover markers to survey the acute changes of bone physiology.13
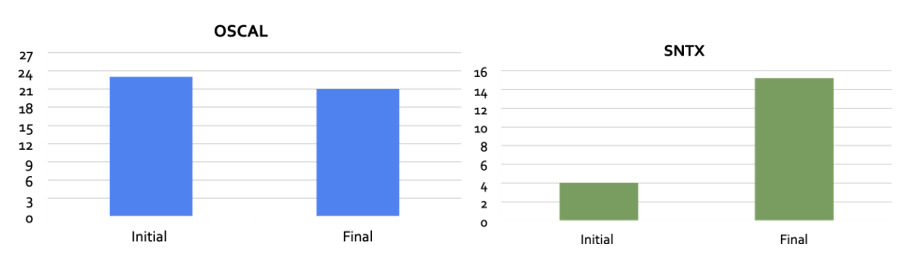
Initial serum markers of serum osteocalcin (OSCAL) and serum N-telopeptide (SNTX) were drawn. Prior to treatment, OSCAL and serum SNTX were 23 ng/mL and 4.0 nM BCE/L, respectively. Following treatment, OSCAL was 21 ng/mL and SNTX was 15.2 nM BCE/L (Figure 1).
DISCUSSION
Human bone is in a constant state of remodeling and turnover.14 Bone is broken down and resorbed by osteoclasts and minerals are deposited by osteoblasts. The byproducts of these cellular activities can be measured via different bone turnover markers (BTM). The aberrant process of bone remodeling leads to a state of low bone mineral density, which has implications on the quality of life and activities of daily living of those affected. Both Osteocalcin (OSCAL) and serum N-telopeptide (SNTX) are markers commonly utilized to monitor bone activity .
OSCAL is a marker used to monitor antiresorptive therapy which looks at the osteoblastic activity. SNTX level is used to monitor the resorptive and osteoclastic activities in bone.15 The changes in serial values of SNTX observed in the patient we report on could indicate that we were able to affect bone metabolism and the remodeling process on a cellular level. The increase in SNTX from 4.0 nM BCE/L to 15.2 nM BCE/L suggests that OMT may be effective in stimulating the initial phase of bone resorption.
It is our assumption that the observed decrease in OSCAL from 23 ng/mL to 21 ng/mL after OMT is due to a complication with the particular marker or the OMT techniques performed. A literature review performed after this finding16 reports that OSCAL is less sensitive for acute changes in bone physiology, and is more reflective of osteoblastic changes that occur weeks to months after the initial resorption process is completed. Furthermore, there are fluctuations associated with the circadian nature of OSCAL that have been extensively described in the literature,17 which limited its use. Further testing might have included other bone turnover markers (BTM) that are more sensitive to the acute bone remodeling changes including Bone Specific Alkaline Phosphatase. BSAP is the only urine marker that has been shown to be independent of circadian fluctuation.18
CONCLUSION
WBA has been notably effective in attenuating bone loss in post-menopausal women, but it provides a number of challenges. Its use is limited by compliance, availability, cost, safety, and feasibility to be self-administered. Through an osteopathic perspective, we replicated the benefits of WBA in the treatment of this post-menopausal patient who presented with back pain.
As our case report followed a single patient, further research is needed to validate our findings in a study that might expand parameters such as the number and types of patients. For example, to include a representative cohort of multinational origin and to include a spectrum of bone mineral density levels via screening bone densitometry. Furthermore, we hope our study will report on functional variables such as improvements in range of motion, quality of life, proprioception, and balance which would decrease the risk of falls and therefore fractures.