Introduction
An aneurysm is defined as a focal dilatation of a blood vessel wall involving all three vascular wall layers: tunica intima, media, and adventitia. Pulmonary artery pseudoaneurysm (PAP) is a focal dilatation of the pulmonary artery caused by leakage of blood through inner layers and contained by adventitia or perivascular soft tissue.1 Malignancy is a rare cause of PAP and is reported in several types of malignancies: metastatic sarcoma, synovial sarcoma of the right atrium, breast cancer, atrial myxoma, squamous cell carcinoma, malignant histiocytoma, angiosarcoma of soft tissue in the neck.2 Here we present the case of a fifty-six-year-old female admitted with a one-week history of progressive dyspnea and a five-month history of menorrhagia and weight loss; extensive workup revealed leiomyosarcoma of the uterus with pulmonary metastases. Herein, we discuss the case of a PAP originating from metastatic leiomyosarcoma of the uterus.
Case Presentation
The patient was a fifty-six-year-old female with no known past medical history who presented with a one-week complaint of progressively worsening dyspnea while on a two-week vacation from her home country. One month prior she developed a dry cough and was prescribed steroids and antibiotics by her primary care physician; however, the cough persisted. She noted five months of menorrhagia which she attributed to her recent diagnosis of uterine fibroids four months prior, and a ten-pound weight loss attributed to her new diet. She denied fever, chills, nausea, vomiting, known sick contacts, and chest pain. On admission lab results showed microcytic anemia, thrombocytopenia, leukocytosis, elevated inflammatory markers, and transaminitis (Table 1). Chest x-ray on admission showed multiple pulmonary lesions scattered throughout the lung fields consistent with metastatic disease and right pleural effusion.
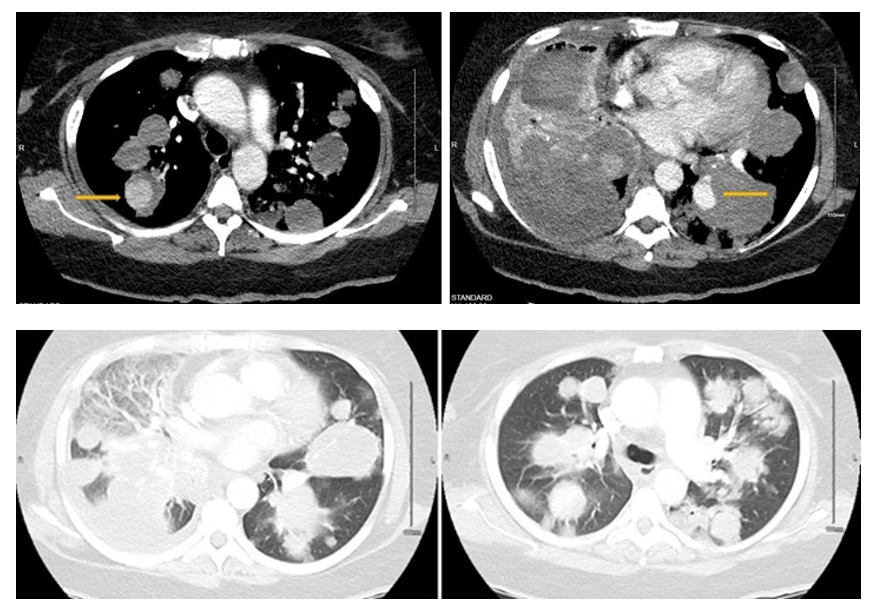
Computerized tomography angiography (CTA) showed multiple bilateral pulmonary nodules, also known as “cannonball appearance,” measuring up to 6.3 cm throughout the lungs consistent with diffuse pulmonary metastases (Figure 1). Upon admission, the patient was alert, awake, and oriented in time and space, febrile at 37.7℃, with a blood pressure of 163/95 mmHg, heart rate of 118 bpm, respiratory rate of 24 with an oxygen saturation of 97% on room air. A physical exam demonstrated a middle-aged female with increased respiratory rate and diminished breath sounds diffusely with absent breath sounds in the right middle and lower lobe on auscultation. The patient was admitted under the impression of dyspnea in the setting of diffuse bilateral pulmonary metastasis.
There was a high suspicion of pulmonary metastases originating from the uterus given a five-month history of menorrhagia. Tumor marker lab value results showed elevated cancer antigen 125 and human epididymis protein 4 ovarian cancer (Table 2). CT abdomen and pelvis showed a multi-fibroid uterus with concern for cervical or endometrial malignancy, enlarged left external iliac lymph node of 1.4 x 2.0 cm, and metastatic disease in bilateral lung bases including a loculated right-sided pleural effusion (Figure 2). Pelvic and transvaginal ultrasound showed an enlarged 40 weeks in size heterogeneous uterus with suspected fibroids.
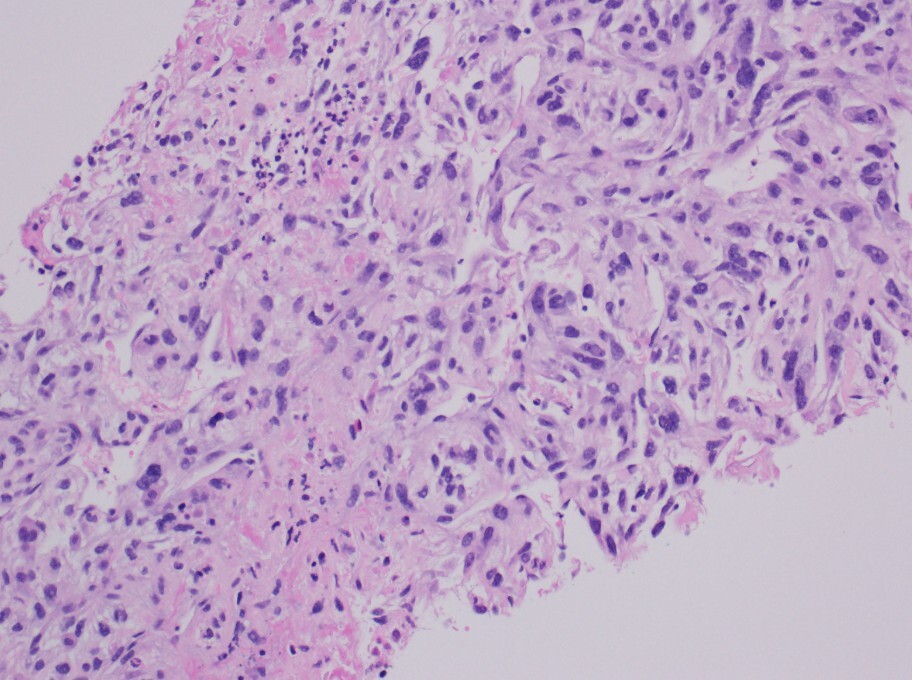
Endometrial biopsy pathology showed endometrial breakdown. Pelvic magnetic resonance imaging (MRI) showed uterine fibroids and a cystic mass with internal solid enhancement peripherally suspicious for malignancy such as leiomyosarcoma (Figure 3). Interventional radiology guided biopsy was performed and pathology revealed poorly differentiated malignant neoplasm of uncertain origin, most likely poorly differentiated leiomyosarcoma and less likely high-grade endometrial stromal sarcoma (Figure 4). The oncology team discussed the prognosis with the patient who agreed to begin chemotherapy with Gemcitabine and Docetaxel with the intention of symptom relief.
Leukocytosis was present throughout the hospital course, ranging from 18.56 to 28.0x10 mcL. Urinalysis was positive for leukocyte esterase, white blood cells, and red blood cells. Urine culture grew Enterococcus, and the patient was treated with Metronidazole for four days and Zosyn for five days. The patient denied dysuria, frequency, and urgency. Given persistent leukocytosis, antibiotics were switched to Augmentin for a total of three days. After antibiotic treatment, leukocytosis persisted and was determined to be most likely reactive and secondary to malignancy. The patient’s hemoglobin decreased from 6.5 to 5.9 g/dL throughout admission and she received 3 units of packed red blood cells.
The patient was hypoxic throughout the hospital course which progressively worsened due to increased tumor burden. She was escalated from two two-liter nasal cannula to bilevel positive airway pressure (BIPAP) within a two-hour window. Repeat CTA twelve days after the admission was negative for pulmonary embolism but showed significant worsening of the cannonball metastases, pneumonia, a pseudoaneurysm measuring 2.5 cm in the left lower lobe within a pulmonary mass, and second pseudoaneurysm or intratumoral hemorrhage within the right upper lobe (Figure 5 and 6). In light of their worsening clinical status and widespread metastatic disease, no interventional option was suitable for the pseudoaneurysm, and since she is no longer qualified for chemotherapy, a decision to initiate palliative care was made. The lower extremity duplex was negative for deep venous thrombosis. The patient was transferred to the step-down unit under the impression of acute hypoxic respiratory failure requiring BIPAP ventilation in the setting of metastatic leiomyosarcoma with likely hospital-acquired pneumonia.
The patient continued to be in respiratory distress which improved with morphine. Analgesia was held to have a family conversation in regards to prognosis and the patient ultimately decided to update her status to do not resuscitate or intubate (DNR/DNI). Two days later, the patient’s mean arterial pressure (MAP) was recorded in the low fifties. She received peripheral norepinephrine to maintain her blood pressure. Despite optimal medical treatment, the patient continued to deteriorate demonstrating tachypnea, progressive bradycardia, and no improvement in MAP. The patient died in the middle of the night. As per the family’s wishes, no aggressive measures such as compressions or intubation were made.
Discussion
PAP is an exceptionally rare clinical entity and typically arises from infections.2 Other etiologies include traumatic, iatrogenic, vasculitis (Behcet’s disease and Takayasu arteritis), and neoplasia.1,2 In the setting of malignancy, PAPs mostly occur in the setting of primary cancer of the lungs.2,3 As squamous cell carcinoma of the lung is associated with necrosis, central cavitation, and direct invasion with necrosis of the vascular wall, it is the most common malignant cause of PAP.1 Metastatic neoplasms-induced PAP is reported in several types of malignancies: metastatic sarcoma, synovial sarcoma of the right atrium, breast cancer, atrial myxoma, squamous cell carcinoma, malignant histiocytoma, angiosarcoma of soft tissue in the neck.2 Primary lung cancers and iatrogenic causes of PAP from tumor treatment were excluded from our literature review (Table 1). Multiple PAPs have only been reported in metastatic sarcoma and atrial myxoma.2 Most PAPs occur peripherally, with 83% found in segmental or subsegmental branches.3
Pathophysiology of PAP in malignancy is complex and includes mechanisms such as local invasion, tumor emboli, or treatment used for the neoplasia.2 The embolized neoplastic cells directly infiltrate the vascular subintimal wall, causing its erosion and loss of normal vascular integrity, resulting in pseudoaneurysm formation.2,3 Prompt diagnosis is essential because of the potential for enlargement and rupture, causing fatal hemoptysis if left untreated in more than 50% of the patients.3
Chest radiography may reveal nonspecific findings such as focal lung consolidation, dense pulmonary infiltrate with hazy margins, or a solitary well-circumscribed nodule.4 CT angiography, with CT pulmonary angiogram protocol, is the diagnostic investigation of choice, as it superiorly characterizes the pseudoaneurysm, including the anatomy of the pathological vessel and surrounding tissues.3 PAP is typically seen as a centrally enhancing, rounded pulmonary nodule with an adjacent vessel that is isodense to the central pulmonary artery.1 However, CT angiograms often underestimate the size of the aneurysm due to the slow filling of the aneurysm with contrast and the presence of an intra-aneurysmal thrombus.1 Anatomic information obtained from pulmonary CT angiography guides selective catheter angiography with endovascular interventions, including direct coil embolization, stent placement, or embolization of the feeding vessel, for occluding pseudoaneurysms is considered the treatment of choice.4 Rarely, operative repair is required with pulmonary resection or direct pulmonary arteriography, i.e., arterial surgical suturing.1 However, most patients are generally too ill with reduced pulmonary functions, especially with metastatic cancers; therefore, pulmonary resection is typically avoided, and observation or interventional techniques are preferred.3
Complications of endovascular treatment include misplaced coils, migrating coils, delayed bacterial contamination, distal pulmonary infarction, and damage to the vessel wall.1
However, even with effective treatment, the prognosis remains poor, with survival rates of 67% and 46% at 1 and 3 months, respectively, reported in the literature.5
Conclusion
We have presented the case of a fifty-six-year-old female with two peripheral PAPs secondary to metastatic leiomyosarcoma of the uterus. Only two of the aforementioned cases were secondary to uterine leiomyosarcoma, making our patient the third known case. Our patient’s clinical deterioration and worsening dyspnea were likely attributed to the progression of pulmonary metastases and hospital-acquired pneumonia. Surgical intervention would not have been suitable for our patient, as her metastatic cancer was too advanced with poor pulmonary reserve and prognosis.

.jpeg)
.jpeg)



.jpeg)
.jpeg)