Introduction
The introduction of highly active antiretroviral therapy (HAART) marks an era of drastically lower cancer rates for people infected with the human immunodeficiency virus (PLWH).1,2 Although most acquired immunodeficiency syndrome (AIDS)-defined cancers (ADCs) became less frequent among this population, the rate of some non-AIDS-defined cancers such as lung cancer, anal cancer, liver cancer, and Hodgkin lymphoma has increased steadily.3,4
A blend of lifestyle, social, and infectious risk factors plays a role in the increased risk of NADCs found in PLWH. An example of this complex interplay is the link between Epstein–Barr virus (EBV) and HL; EBV infection in combination with the B cell hyperstimulation response resulting from HAART-related immune reconstitution leads to an uncontrolled proliferation of infected B cells. Another example is the relationship between (Human Papilloma Virus) HPV infection and anal cancer, both of which are more frequent in Men Who Have Sex with Men (MSM) or those who perform anal sex. Additionally, with HAART being ineffective against HPV, and PLWH nowadays living longer, the incidence of anal cancer in this coinfected population has increased. Finally, Immune dysfunction resulting in persistent latent infection and reduced immunosurveillance are also risk factors in carcinogenesis.4,5
Among men and women, colorectal cancer (CRC) is ranked as the third cause of cancer – related death worldwide, leading to financial and public health burdens.5 Thus, it is imperative that we fully identify the risk factors of CRC in vulnerable populations, such as PLWH. Conflicting studies exist regarding the risk of CRC in PLWH.
In a prospective study done by Patel et al., 54,780 HIV-infected persons in the United States were followed from 1992 to 2003 and standardized rate ratios for multiple cancers were calculated to compare their incidence in the HIV-infected population with that in the general population. The incidence of colorectal cancer was higher in the HIV-infected population than in the general population with a SIR of 2.3 [CI, 1.8 to 2.9].5
Conversely, Coghill et al. collected incident colorectal cancer in 713 PLWH using data from the HIV/AIDS Cancer Match Study (1996–2012). Comparisons with general population cancer rates using standardized incidence ratios (SIRs) showed a reduced CRC risk in PLWH including proximal colon, distal colon, and rectum with the following respective SIRs (0.67, 95% CI [0.59 to 0.75], P < .001; 0.51, 95% CI [0.43 to 0.59], P < .001; and 0.69, 95% CI [0.61 to 0.77], P < .001).6
Interestingly, Silverberg et al. performed a cohort study of 20,775 HIV-infected and 215,158 matched HIV-uninfected Californians from 1996 to 2008, and obtained the Adjusted rate ratios (RR) for HIV status of different cancers. There was no increased risk for colorectal (RR=0.9; P=0.34).7
In a comprehensive review performed by Kan et al, the age-adjusted standardized incidence ratio (SIR) of CRC in the HIV-positive and/or AIDS patient population ranges from 0.33 to 3.6.8
Although most studies demonstrate either decreased or no significant difference in the incidence of CRC between PLWH and patients without HIV infection, Patel et al showed that PLWH were at higher risk.5,9,10
We undertook this study to further elucidate the risk factors associated with CRC in PLWH. By understanding individual risk factors in PLWH, providers can tailor CRC screening guidelines, with the goal of early intervention and improved patient survival. We hope that this study sheds light on the importance of early detection of CRC in such a vulnerable population.
Materials And Methods
Database
Data was collected from the electronic medical record-based commercial database: Explorys Inc, Cleveland, OH, USA. Cleveland, OH, USA; an aggregate of electronic medical records data from 26 major integrated US healthcare systems consisting of 36 US hospitals, of patients > 18 years old, between 2015 and 2020. Explorys contains de-identified data sourced from electronic medical records across all institutions that participate. This data undergoes collection, standardization, and storage within a cloud-based system. Unlike the widely used International Classification of Diseases codes, Explorys employs the Systematized Nomenclature of Medicine - Clinical Terms (SNOMED-CT) for diagnoses. Utilizing SNOMED-CT diagnoses allows for the extraction of data from Explorys across different groups, which can then be further divided into smaller groups by utilizing additional diagnoses or applying diverse filters, such as different demographic characteristics. To safeguard patient confidentiality, the database research engine rounds population counts to the nearest 10, treating all counts between zero and 10 as equivalent. Given its reliance on de-identified data, this database aligns with Health Insurance Portability and Accountability Act (HIPAA) standards, rendering institutional review board approval unnecessary for studies utilizing this database.
Study design
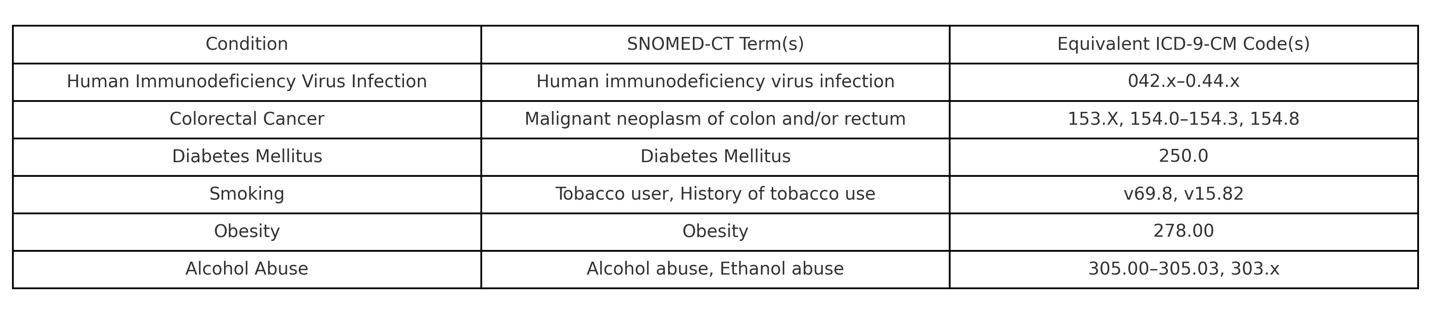
We performed a retrospective cohort analysis, which included all active medical records between the years 2015 and 2020. After excluding all patients under the age of 20 and those with a family history of gastrointestinal tract malignancies, a cohort identified all patients with SNOMED-CT diagnosis of “Human immunodeficiency virus infection”. The control group was then identified as patients without SNOMED CT diagnoses of “Human immunodeficiency virus infection”. Basic demographic information, including age, sex, and race, along with other comorbid conditions were identified in the study and control groups according to the presence or absence of their corresponding SNOMED-CT diagnosis. We contrasted our selected SNOMED CT terms for CRC, HIV, and comorbidities to equivalent ICD-9-CM codes which have been utilized in prior studies using population-based data to identify their respective conditions (Table 1). A multivariate regression analysis model was performed to adjust for confounding factors.
Covariates
Age, sex, and race-based data were collected. Potential confounding factors were also identified including age, sex, race, tobacco smoking, alcohol abuse, diabetes mellitus, and obesity.
Statistical analysis
There were 2 major cohorts: patients with HIV, and patients without HIV. The overall prevalence of CRC was calculated by dividing the number of CRC cases by the total number of hospitalized patients with HIV. Similarly, the prevalence of CRC was also calculated among patients without HIV.
Prevalence was then calculated in smaller groups based on age and race. After the initial univariate analysis, a statistical multivariate model was performed using Statistical Package for Social Sciences (SPSS) version 25.0 (IBM Inc., Armonk, New York) to adjust for the known risk factors. These factors included age, sex, race, obesity, diabetes mellitus (DM), smoking, and alcohol abuse. To adjust for potential confounding from the aforementioned covariates, 512 searches were performed to account for every probability. All statistical analyses were performed using IBM SPSS Statistics version 25, with CRC as an outcome between the HIV group and the control patients without HIV and adjusting for confounding factors. For all analyses, the adjusted odds ratio was calculated with 95% confidence intervals (CIs), and a two-sided p-value of less than 0.05 was considered statistically significant.
Results
Descriptive analysis
There were 217,570 HIV patients (57.3% male; with 86.6% in the age group of 20-64 years) included in this study between the years 2015 and 2020, and 38,898,150 patients without HIV (44.2% male, with 77.9% in the age group of 20-64 years) in the control group. A power analysis for proportion was performed using the method described by Naing et al. (2022). The calculated sample size required to detect a CRC prevalence of 0.16% with a margin of error of 0.0005 was approximately 12.288. Since our study population greatly exceeded this number, it ensured sufficient power for precise prevalence estimates and subgroup analyses. Patients with HIV had a higher prevalence of comorbidities compared with control patients, including smoking status (25% vs 13.3%), alcohol abuse (4.8% vs 1.8), obesity (5.8% vs 3.9%), and diabetes mellitus (23.2 % vs 10.2%). (Table 2)
In both groups, most of the patients were of the Caucasian race (63.2% vs 60.2%) whereas Hispanic/Latino was the least category (2.2% vs 6.4%). A higher percentage of patients with HIV were African American compared to those without HIV (19.4% vs. 11.2%), while the opposite was observed for patients categorized as belonging to other races (15.2% vs. 22.2%). (Table 2)
Table 2: Baseline characteristic of the study population. It provides demographic and medical information of a population of 217,570 individuals with HIV and 38,898,150 individuals without HIV. The variables listed in the table include age, sex, race, and medical comorbidities.
Prevalence
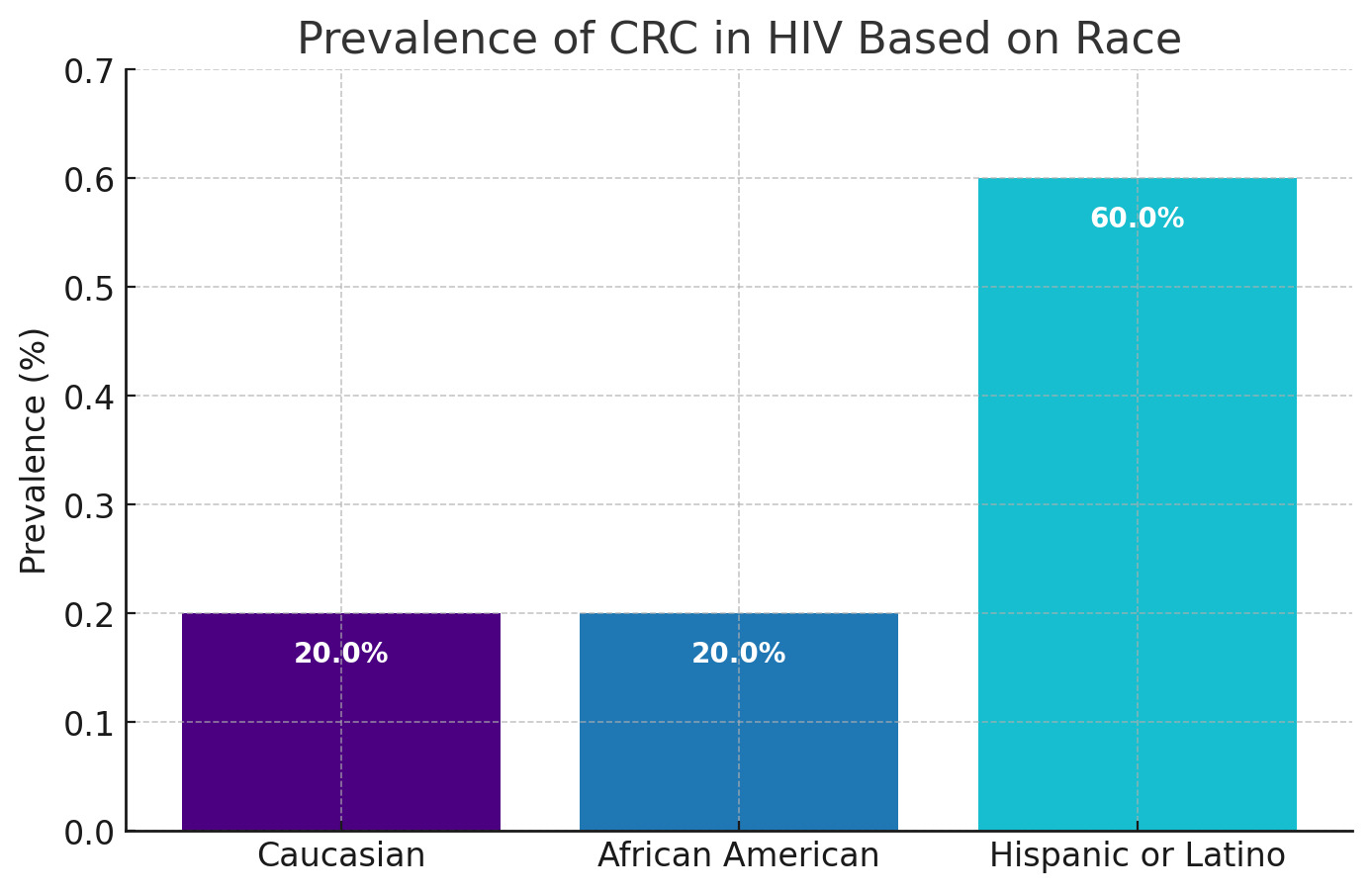
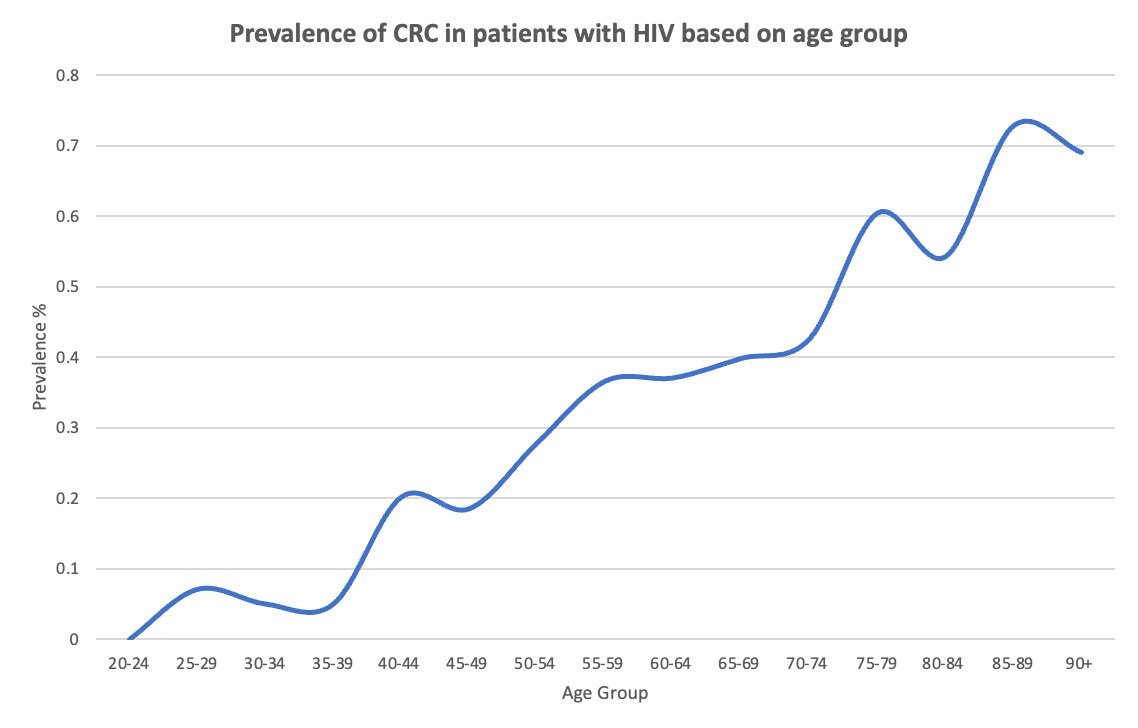
The prevalence of CRC in individuals living with HIV was 0.16%, indicating a twofold increase when compared to HIV-negative patients, who had a prevalence of 0.08%. This disparity was statistically significant (P < 0.0001). Prevalence of CRC in HIV-positive Hispanics or Latinos was 0.62% whereas in Caucasians and African Americans, it was almost the same around 0.17% (Figure 1). The prevalence of CRC in HIV-positive patients based on age group is in Figure 2 which shows an overall proportional increase in prevalence of CRC concerning age except for a small drop in the 80 – 84 age group.
Multivariate Regression Analysis
In the multivariate model, after adjusting for age, sex, race, tobacco smoking, alcohol abuse, diabetes mellitus, and obesity, HIV-positive patients were more likely to develop CRC with OR 1.796 (95% CI 1.712-1.883, P < 0.0001) compared to HIV-negative individuals. This indicates that HIV-positive individuals have approximately an 80% increased risk of developing CRC. In contrast, the odds for developing CRC in Caucasians patients notably higher with an OR of 6.363 (95% CI 6.296-6.431), indicating that Caucasian patients were approximately 536% more likely to develop CRC compared to non-Caucasians.
The odds for developing CRC were higher among Male patients OR 1.795 (95% CI 1.776-1.815, P < 0.0001) than female patients, elderly specifically aged above 65 years OR 1.174 (95% CI 1.163-1.185, P < 0.0001) than patients younger than 65 years, patients who drink alcohol OR 1.661 (95% CI 1.636-1.687, P < 0.0001) than non-alcoholics, patients who smoke OR 1.712 (95% CI 1.692-1.732, P < 0.0001) than nonsmokers, obese patients with BMI>30 OR 1.477 (95% CI 1.460-1.495, P < 0.0001) than patients with BMI <30 and finally patients with diabetes mellitus OR 1.560 (95% CI 1.520-1.602, P < 0.0001) than non-diabetics. (Table 3)
Table 3: Multivariate Regression Analysis with CRC Being the Outcome. It presents a comparison of an outcome (CRC) among different groups including HIV positive vs negative, Caucasians vs non-Caucasians, male vs female, age >65 vs <65, alcoholics vs non-alcoholics, smokers vs non-smokers, obese vs non-obese, and finally diabetics and non-diabetics.
Discussion
HIV infection has traditionally been thought to confer an increased risk of cancer.1 Although the introduction of HAART treatment has improved the cancer rates found in PLWH, patients with HIV continue to suffer from higher rates of malignancy when compared to the rest of the population.1,10
Several mechanisms are responsible for the higher rates of cancer in PLWH. HIV- related immunosuppression allows oncogenic viruses to thrive, creating an environment of chronic inflammation conducive to premature carcinogenesis.1,11 Social factors such as access to screening and behavioral risks may also play a role in cancer formation.1 Social behaviors in PLWH, such as anal sex in MSM, can also predispose patients to co-infection with oncogenic viral infections, including HPV and EBV.1 Increased lifespan of PLWH after HAART can also play a role in the increasing rates of cancer, as patients live longer allowing these malignancies to be discovered.12,13
Malignancies in HIV-infected patients are defined as NADC (Non-AIDS Defining Cancers) or ADC (AIDS Defining Cancers).1 ADCs are typically a result of chronic, oncogenic viral infection in the setting of HIV-related immunosuppression.1,10 ADCs encompass Kaposi sarcomas, certain cervical cancers, and non-Hodgkin’s lymphoma.1 NADCs are further subcategorized into viral (typically oncoviral) and nonviral malignancies.1 Viral NADCs include hepatocellular carcinoma (associated with Hepatitis B and Hepatitis C infection), Hodgkin lymphoma (associated with Epstein-Barr infection), and cancers associated with Human Papilloma Virus (HPV).1 Nonviral NADCs encompass stomach, colorectal, prostate, and many other solid cancers.1
After the introduction of Highly Active Antiretroviral Therapy (HAART) in the 1990s, the incidence of AIDS-defining conditions (ADCs), specifically in people living with HIV (PLWH), has significantly decreased.1,9,10 However, the rates of NADCs have increased steadily over this time.1,10,13 PLWH continues to suffer from an overall higher risk of cancer compared to the general population.1 Paradoxically, certain NADCs (colorectal cancer in particular) have been reported to occur at lower rates in patients with HIV.1,10 We undertook this study to specifically understand the prevalence of colorectal cancer in patients with HIV infection. Understanding the incidence of colorectal cancer and its associated risk factors in this specific population can help tailor screening guidelines in this PLWH.
The literature regarding the prevalence of CRC in PLWH is mixed, with studies suggesting both increased and decreased risk compared to the general population.8,10,13 According to Kan et al., the literature regarding the incidence of CRC in PLWH in multiple countries (including France, Swiss, UK, US, Australia) showed that the majority of studies conducted reported either a lower or a non-significant change in CRC incidence compared to the general population.6–8
Our study shows a 0.16% higher risk of CRC in patients with HIV. In contrast, in a large observational cohort study conducted by Lam et al., 3177 PWLH and 29,219 Californians without HIV were included. The results of this study showed that the prevalence of CRC was 0.5% in PLWH and 1.0% in persons without HIV. There was no difference in the prevalence of either adenoma or CRC by HIV status in adjusted analyses.14
Similarly, a meta-analysis of independent studies conducted by O’Neill et. al. found no change in the risk of CRC and colon cancer between HIV-infected and non-HIV-infected individuals (note: this study excluded individuals with rectal cancer).10 However, when pooled data of CRC and colon cancer were assessed separately, it was found that PLWH had a lower risk of colon cancer.10 O’neill et al also showed that after pooling the results from 3 studies, there was an increased risk of CRC among women.10 Our study did not distinguish between CRC and colon cancer, and it would be interesting to study whether the two-fold higher risk of CRC would change if the study sub-categorized CRC and colon cancer. The reliability of these studies was questioned because of the low number of patients and the presence of significant heterogeneity. In our study, although there was a male predominance in both groups and there was an increased risk of CRC in male patients, but we did not study the latter in the HIV group specifically. Only a few other studies that showed significantly increased risk of CRC in the HIV population akin to our study.5,15
Certain theories have been proposed that could explain this fact such as HIV-1 viral proteins and molecules could impact cell survival.1 HAART therapy itself has been suggested to contain some level of antitumor activity.1 The PI (proteasome inhibitor) class of HAART drugs, for example, has shown inhibition of cell survival via PI3K/AKT pathways.1 NRTIs (nucleoside reverse transcriptase inhibitors) are suggested to inhibit DNA replication in tumor cells.1 However the increased risk of CRC found in our study suggests that perhaps CRC may have mechanisms of overcoming these antitumor pathways. Future molecular studies of CRC biopsies in PLWH could help shed light on whether the risk of CRC in PLWH is truly reduced compared to the general population.
Individuals with HIV infection may have predisposing social factors that can increase the risk of CRC. Smoking tobacco and alcohol use, for example, has been associated with an increased risk for malignancies.1,8,12 Our study found that patients with HIV infection had higher rates of smoking (25% compared to 13.3% in the non-HIV population) and higher rates of alcohol abuse (4.8% compared to 1.8%) in the general population. Although our study cannot suggest a causal relationship between these risk factors and CRC, our results suggest that HIV-infected patients are more vulnerable to these lifestyle risks. A retrospective study by Mills et. al did establish a relationship between tobacco and alcohol, and CRC.12 They found that PLWH who had CRC were more likely to report tobacco and alcohol use when compared to patients with CRC alone.12
Obesity is another lifestyle risk factor that contributes to the risk of CRC. In our study, PLWH with a BMI >30 was at higher risk (OR 1.477, p > 0.0001) of CRC. These findings are consistent with what is currently reported in the literature. A study by Mills et. al. also found that patients with HIV infection and CRC had an overall lower BMI, when compared to patients with CRC alone.11 Similarly, Kelly et al demonstrated a positive correlation between adherence to physical exercise and CRC screening.12 There was also a negative correlation between obesity and the likelihood of CRC screening.12 Although these results were based only on African American men with HIV, these findings suggest a social link between a patients’ tendency to partake in physical activity and adhere to screening suggestions. While our study did not assess the relationship between HIV infection and BMI, our results suggest that increased BMI alone may be a risk factor for CRC.
Expectedly, our study demonstrated that patients >65 years of age had a higher risk of developing CRC. Notably, Mills et al found that patients with HIV infection developed CRC almost a decade earlier (mean age 51.3) than the general population.12 This can be explained by the earlier onset of precursor lesions in patients with HIV infection. Colonic adenomatous polyps are precursor lesions to CRC and have been reported to be increased in patients with HIV.8,10 Further studies should be conducted to assess the relationship between HIV status and colonic polyps, and whether there is an associated risk in progression to CRC. Discovering polyps early in the carcinogenic process can allow for timely intervention and improved outcomes, particularly in younger PLWH. General screening guidelines are not currently tailored to immunocompromised populations. Although initially, Keller et al’s. data results showed that PLWH were more likely to have received screening for colorectal cancer, after adjusting for comorbidity index and years in the dataset, the converse holds true; PLWH are actually less likely to get CRC screening.9 This was also corroborated by other studies that showed that PLWH were less likely to receive CRC screening than the general population.16
Population Comparison and Prevalence Differences
The population characteristics of our study sample may help explain the observed differences in CRC prevalence compared to prior studies. Our dataset, derived from the Explorys database, included a higher proportion of individuals with known risk factors for colorectal cancer, such as smoking (25% in HIV-positive vs. 13.3% in HIV-negative individuals), alcohol abuse (4.8% vs. 1.8%), and obesity (5.8% vs. 3.9%). These elevated rates of lifestyle-related risk factors could contribute to the increased CRC prevalence seen in our HIV-positive cohort. Additionally, our dataset contained a larger proportion of African Americans (19.4% vs. 11.2%) compared to the general population. Since African Americans have a higher baseline risk for CRC, this demographic skew may further explain the heightened CRC rates we observed. Compared to studies like those by Patel et al., Coghill et al., and Silverberg et al., which analyzed diverse populations with varied demographic distributions and lifestyle factors, our sample’s higher concentration of known CRC risk factors may have contributed to the differing prevalence rates. These distinctions highlight the importance of accounting for population differences when interpreting CRC prevalence in PLWH populations.
Limitations
Although we found a significantly increased risk of CRC in PLWH, our study did have limitations. For example, we did not assess individual components of the immune system and their relationship with CRC. One of the proposed mechanisms of CRC pathogenesis is immune suppression. And this was corroborated by studies showing that a low CD4 count was associated with an increased risk of CRC.4,13 We were not able to identify CD4 counts and their relation to CRC prevalence. Additionally, we had to rely on the SNOMED-CT codes, therefore, we cannot verify the accuracy of the diagnosis, and there is also the possibility of coding errors. Another limitation is that temporal relationships cannot be established by using our study. Similarly, this is an observational study; therefore, it is difficult to truly establish prevalence and establish a causal relationship for a risk factor. Also, some variable stratifications (for example age) criteria were set by Explorys, and due to the statistical methods used with the database, N= 10 patients were unaccounted for in the HIV population when stratified by gender. These figures were rounded up to equate with the total, with negligible impact on the overall percentage. Finally, we did not assess overall mortality from CRC within this population.
Conclusion
This study contributes valuable insights into the heightened risk of colorectal cancer (CRC) within the HIV population, a phenomenon not widely explored in existing literature. Our findings underscore the necessity for potential adjustments in screening guidelines to cater to this demographic. Given the elevated prevalence of adenomatous polyps among HIV patients, early detection through tailored screening protocols holds promise for mitigating malignant progression and enhancing survival outcomes.
However, comprehensive understanding of CRC risk in this population necessitates further investigation, particularly regarding its correlation with CD4 counts. Continued research efforts are important to elucidate further associations between HIV infection, immune status, and colorectal malignancy, thereby informing more targeted prevention and management strategies.